Adhesive capsulitis, often known as frozen shoulder, is a painful condition. It limits movement in the shoulder joint.
Many people wonder about its connection to diabetes. Research shows that individuals with diabetes are at a higher risk for developing adhesive capsulitis. This relationship raises important questions about management and treatment. Understanding how these two conditions interact can help both patients and healthcare providers.
People with diabetes should be aware of the symptoms of frozen shoulder. Early detection can lead to better outcomes. We will explore the links between adhesive capsulitis and diabetes. We will discuss symptoms, risk factors, and possible treatment options. By the end, you will have a clearer picture of this important health topic.
Adhesive Capsulitis: A Brief Introduction
Adhesive capsulitis, often known as frozen shoulder, is a condition that restricts shoulder movement. It can cause significant pain and stiffness. This condition often links to diabetes. Understanding adhesive capsulitis is important for effective treatment.
What Is Adhesive Capsulitis?
Adhesive capsulitis is a painful condition that affects the shoulder joint. It results in a thickening and tightening of the shoulder capsule. This capsule surrounds the shoulder joint. The cause is not always clear. However, it often develops after injury or surgery.
This condition typically progresses through three stages:
- Freezing Stage: Pain increases and range of motion decreases.
- Frozen Stage: Pain may lessen, but stiffness remains.
- Thawing Stage: Range of motion improves gradually.
Symptoms And Diagnosis
Symptoms of adhesive capsulitis include:
- Shoulder Pain: Often severe, especially at night.
- Stiffness: Difficulty in moving the shoulder.
- Limited Range of Motion: Trouble lifting the arm.
To diagnose adhesive capsulitis, healthcare providers often use:
- Patient history and physical examination.
- X-rays to rule out other issues.
- Magnetic resonance imaging (MRI) for detailed images.
Understanding these symptoms and diagnostic methods helps in early intervention.
Diabetes Mellitus: The Basics
Diabetes Mellitus is a condition that affects how the body uses sugar. This sugar, called glucose, is important for energy. People with diabetes cannot manage glucose properly. This can lead to serious health issues. Understanding diabetes helps in managing its effects.
Types Of Diabetes
There are three main types of diabetes:
| Type | Description |
|---|---|
| Type 1 Diabetes | This type occurs when the body does not produce insulin. |
| Type 2 Diabetes | This type happens when the body cannot use insulin properly. |
| Gestational Diabetes | This type occurs during pregnancy and usually goes away after. |
Each type has different causes and treatments. Understanding these types is important for managing diabetes.
Long-term Health Implications
Diabetes can lead to many long-term health problems. Here are some common issues:
- Heart Disease: High blood sugar increases heart risks.
- Nerve Damage: This can cause pain and numbness.
- Kidney Damage: Diabetes can harm kidney function.
- Eye Problems: It can lead to vision loss and blindness.
Managing diabetes is crucial. Regular check-ups help prevent these problems. A healthy diet and exercise also play a vital role.
Correlation Between Diabetes And Adhesive Capsulitis
Adhesive capsulitis, often known as frozen shoulder, is a painful condition. It limits shoulder movement. Studies show a strong link between adhesive capsulitis and diabetes. Understanding this connection helps in managing both conditions.
Prevalence In Diabetic Patients
Frozen shoulder is more common in people with diabetes. Research indicates that:
- 10% to 20% of diabetic patients may develop adhesive capsulitis.
- Women are affected more than men.
- Diabetes duration increases the risk of shoulder problems.
In diabetic patients, the risk increases with age. Older adults face higher chances of developing this condition. The prevalence is significant, especially for those with type 1 or type 2 diabetes.
Risk Factors
Several factors contribute to the risk of adhesive capsulitis in diabetic patients. These include:
- Duration of Diabetes: Longer diabetes duration raises the risk.
- Blood Sugar Levels: Poorly controlled blood sugar increases the likelihood.
- Age: Older adults have higher chances of frozen shoulder.
- Gender: Women are more prone to this condition.
- Other Health Conditions: Thyroid disorders or heart disease can increase risk.
Understanding these factors helps in early detection. Early intervention can reduce the severity of adhesive capsulitis.

Credit: www.centerfororthosurgery.com
Pathophysiology Behind The Connection
Adhesive capsulitis, commonly known as frozen shoulder, is linked to diabetes. Understanding this connection helps explain why many diabetic patients develop this painful condition. The pathophysiology involves complex interactions between glucose levels and connective tissue health.
Effects Of Hyperglycemia On Connective Tissue
Hyperglycemia, or high blood sugar, affects body tissues. It changes the structure and function of connective tissue. Here are key effects:
- Increased Glycation: High glucose levels lead to glycation. This process damages proteins in the connective tissue.
- Loss of Elasticity: Glycated collagen loses flexibility. This stiffness contributes to restricted movement.
- Collagen Cross-Linking: Excess glucose promotes cross-linking in collagen. This makes tissues less pliable.
These changes can lead to inflammation and pain in the shoulder joint. They also hinder recovery from injury.
Inflammatory Response In Diabetic Individuals
Diabetes triggers a unique inflammatory response. This response plays a significant role in adhesive capsulitis. Key points include:
- Higher Cytokine Levels: Diabetic patients often have elevated levels of inflammatory cytokines. These proteins signal inflammation.
- Chronic Inflammation: Ongoing inflammation worsens tissue damage. It increases pain and limits movement.
- Impaired Healing: Diabetes slows down the healing process. This makes recovery from injuries longer.
Understanding these factors helps in managing adhesive capsulitis in diabetic patients. Awareness can lead to better treatment options and improved outcomes.
Clinical Studies On Diabetic Shoulder Conditions
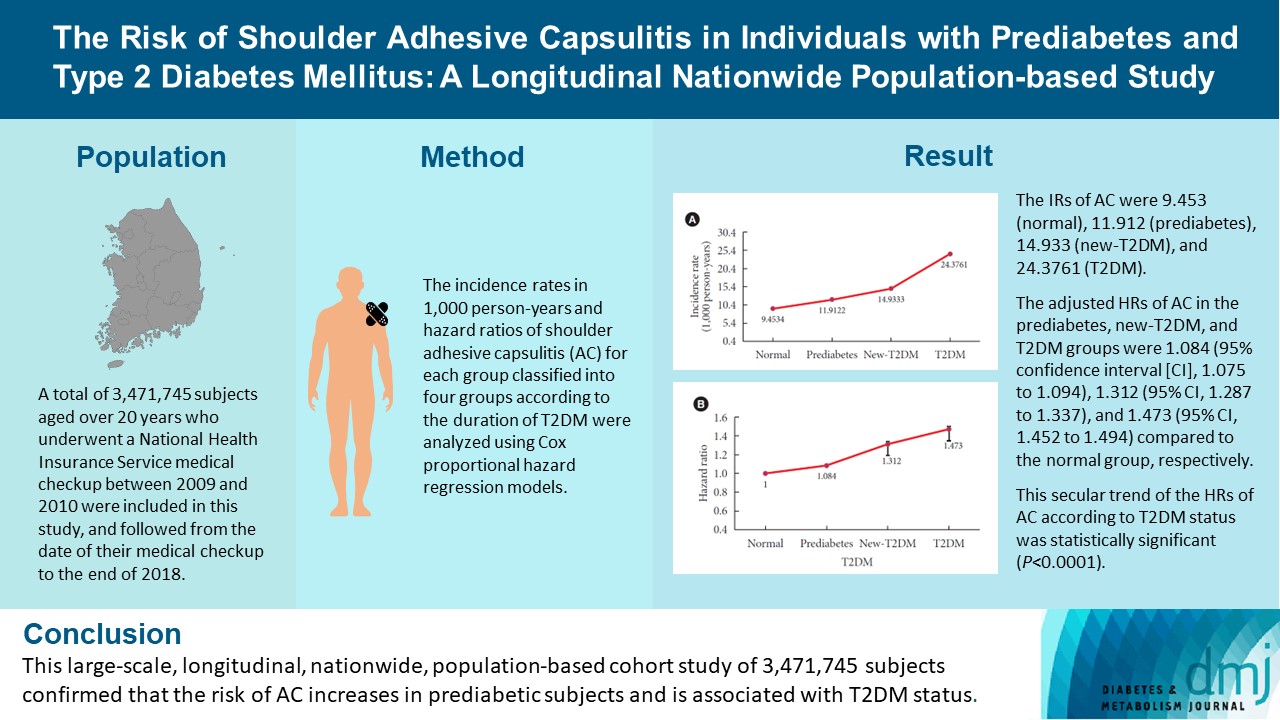
Adhesive capsulitis, often called frozen shoulder, affects many people with diabetes. Clinical studies show a strong link between these two conditions. Understanding this relationship helps in providing better care. Research highlights the prevalence and impact of shoulder issues in diabetic patients.
Research Findings
Many studies explore the connection between diabetes and shoulder pain. Here are some key findings:
- Patients with diabetes have a higher risk of adhesive capsulitis.
- Frozen shoulder occurs more often in women than men.
- High blood sugar levels may worsen shoulder symptoms.
- Diabetic patients often experience slower recovery.
A study showed that about 20% of people with diabetes develop frozen shoulder. This is significantly higher than in the general population. Other research indicates that shoulder stiffness appears more frequently in those with long-term diabetes.
Patient Demographics
Demographic factors play an important role in diabetic shoulder conditions. Here is a breakdown:
| Demographic Factor | Impact on Shoulder Conditions |
|---|---|
| Age | Higher risk in patients over 40 years old. |
| Gender | Women are more affected than men. |
| Duration of Diabetes | Longer duration increases the risk of frozen shoulder. |
| Obesity | Obese patients have a higher chance of shoulder issues. |
Understanding these demographics helps identify patients at risk. This knowledge leads to better prevention and treatment strategies. Early intervention can improve outcomes for diabetic patients with shoulder problems.
Management Strategies For Diabetics With Adhesive Capsulitis
Managing adhesive capsulitis in diabetics requires a careful approach. This condition, also known as frozen shoulder, can be more challenging for those with diabetes. Effective management focuses on reducing pain, improving range of motion, and managing blood sugar levels. Below are key strategies for diabetics dealing with adhesive capsulitis.
Physical Therapy Approaches
Physical therapy plays a vital role in recovery. It helps restore movement and reduce stiffness. A physical therapist can create a tailored program for each patient. Common physical therapy techniques include:
- Stretching exercises to improve flexibility
- Strengthening exercises to support the shoulder
- Manual therapy techniques to relieve pain
- Heat and ice treatments to reduce inflammation
Regular sessions can help track progress. Patients should follow the therapist’s advice and practice exercises at home. This consistency can lead to better outcomes.
Medication And Treatment Options
Medications can help manage pain and inflammation. Common options include:
| Medication Type | Purpose |
|---|---|
| NSAIDs (e.g., ibuprofen) | Reduce pain and swelling |
| Steroid injections | Provide quick relief from inflammation |
| Oral corticosteroids | Manage severe inflammation |
Consult with a healthcare provider before starting any medication. Proper management of blood sugar levels is crucial. Uncontrolled diabetes can worsen symptoms and delay healing. Regular check-ups can help monitor both conditions effectively.
In some cases, surgery may be necessary. Surgical options include:
- Arthroscopic capsular release
- Manipulation under anesthesia
These procedures are less common. They are considered after other treatments fail. Always discuss the risks and benefits with a healthcare professional.
Role Of Blood Sugar Control In Preventing Joint Complications
Adhesive capsulitis, commonly known as frozen shoulder, affects many people with diabetes. The relationship between high blood sugar and joint issues is significant. Controlling blood sugar can help prevent these complications. Understanding glycemic management is essential for better joint health.
Importance Of Glycemic Management
Maintaining stable blood sugar levels is crucial. High blood sugar can cause inflammation and damage joints. This damage can lead to conditions like adhesive capsulitis. Regular monitoring of blood sugar helps in early detection of issues.
Key benefits of good glycemic management include:
- Reduced inflammation in the body.
- Lower risk of joint complications.
- Improved overall mobility and flexibility.
People with diabetes should aim for a blood sugar level between 80-130 mg/dL before meals. The A1C test should be below 7% for optimal health.
Lifestyle Changes For Better Outcomes
Making simple lifestyle changes can improve glycemic control. Here are some effective strategies:
- Regular Exercise: Aim for at least 150 minutes of moderate activity each week.
- Balanced Diet: Focus on whole foods like fruits, vegetables, and whole grains.
- Hydration: Drink plenty of water to stay hydrated.
- Weight Management: Maintain a healthy weight to reduce stress on joints.
Consider working with a healthcare provider. They can help create a plan tailored to individual needs.
In summary, managing blood sugar is vital. It helps prevent joint complications like adhesive capsulitis. Simple lifestyle changes can lead to better outcomes.
Credit: www.e-dmj.org
Surgical Interventions And Their Outcomes
Surgical options can help treat adhesive capsulitis in diabetes patients. These surgeries aim to restore shoulder movement and reduce pain. Understanding the indications and expected outcomes is crucial for patients.
Indications For Surgery
Surgery is not the first option. It is usually considered when other treatments fail. Here are some key reasons for surgical intervention:
- Severe pain that limits daily activities.
- Stiffness that does not improve with physical therapy.
- Persistent symptoms lasting over six months.
Surgeons evaluate the patient’s overall health. They also consider the severity of the condition. A thorough assessment helps in making the best decision.
Recovery And Prognosis
Recovery time varies by individual. It typically lasts from a few weeks to several months. Post-surgery rehabilitation is essential for optimal recovery. Here is a typical recovery timeline:
| Phase | Timeframe | Activities |
|---|---|---|
| Initial Recovery | 1-2 weeks | Rest, pain management, gentle motion exercises |
| Rehabilitation | 2-6 weeks | Physical therapy, strength training, gradual increase in activities |
| Full Recovery | 3-6 months | Return to normal activities, continued exercise regimen |
Most patients see improvements in pain and mobility. The prognosis is generally good for those who follow rehabilitation.
Regular follow-ups with healthcare providers are important. They help monitor progress and adjust treatment plans as needed. This ensures the best outcomes for patients with adhesive capsulitis and diabetes.
Impact Of Adhesive Capsulitis On Quality Of Life
Adhesive capsulitis, also known as frozen shoulder, can greatly affect daily life. It causes pain and limits movement in the shoulder. This condition can be especially challenging for people with diabetes. The impact on quality of life can be significant. Understanding these effects can help in managing the condition.
Daily Living Challenges
Living with adhesive capsulitis brings many daily challenges. Simple tasks become hard or impossible. Here are some common difficulties:
- Reaching overhead: Grabbing items from high shelves is tough.
- Getting dressed: Putting on clothes can be painful and frustrating.
- Driving: Steering a car may cause discomfort.
- Personal care: Brushing hair or bathing can be difficult.
These limitations can lead to a loss of independence. Many people may need help with everyday tasks. This dependency can be hard to accept.
Psychological Effects
Adhesive capsulitis can also affect mental health. Chronic pain often leads to feelings of frustration and sadness. Patients may experience:
- Stress: Managing pain adds to daily stress.
- Anxiety: Worrying about future limitations is common.
- Depression: A feeling of hopelessness can arise.
- Social withdrawal: People may avoid activities with friends.
Recognizing these psychological effects is vital. Support from friends and family can help. Seeking professional help may also be beneficial.
Insights From Endocrinologists And Orthopedic Experts
Adhesive capsulitis, often known as frozen shoulder, affects many people, especially those with diabetes. Understanding this link is crucial for effective treatment. Experts from both endocrinology and orthopedics shed light on this relationship. Their insights help us grasp how diabetes impacts shoulder health.
Expert Opinions
Endocrinologists note that high blood sugar levels can lead to inflammation. This inflammation can stiffen the shoulder joint. They emphasize the need for good blood sugar control. Maintaining stable levels may reduce the risk of adhesive capsulitis.
Orthopedic specialists observe that frozen shoulder occurs more often in diabetic patients. They suggest that diabetes causes changes in connective tissue. This can make the shoulder more prone to stiffness and pain. Treatment plans should include both medication and physical therapy.
| Expert Field | Key Insights |
|---|---|
| Endocrinology | Control blood sugar to reduce inflammation. |
| Orthopedics | Diabetes increases stiffness risk in shoulder joints. |
Multidisciplinary Care Approaches
Addressing adhesive capsulitis requires a team approach. Collaboration between endocrinologists and orthopedic experts is vital.
- Regular monitoring of blood sugar levels.
- Physical therapy to improve shoulder mobility.
- Medication to manage pain and inflammation.
Patients benefit from this combined care. It ensures that both diabetes and shoulder issues are managed effectively. The goal is to restore movement and alleviate pain. Such approaches lead to better outcomes for patients.
Personal Stories: Living With Both Conditions
Living with both adhesive capsulitis and diabetes can be tough. Many people face unique challenges. Their experiences shed light on the impact of these conditions. Here, we share stories from those who live with both.
Patient Experiences
Many patients describe their journey with adhesive capsulitis and diabetes. Here are some real-life experiences:
- Maria, 52: “I felt pain in my shoulder. It made daily tasks hard. Managing my diabetes added stress.”
- John, 47: “I didn’t know my shoulder pain was linked to diabetes. It took time to connect the dots.”
- Lisa, 34: “My doctors told me my diabetes could worsen my shoulder pain. I felt overwhelmed.”
These stories highlight the struggle. Many face a mix of physical and emotional challenges.
Coping Mechanisms
Finding ways to cope is crucial. Here are some strategies that have helped others:
- Physical therapy: Regular sessions help regain shoulder movement.
- Exercise: Gentle exercises can ease pain and improve flexibility.
- Diet management: Eating healthy helps control diabetes and overall health.
- Support groups: Sharing experiences with others provides comfort and advice.
Each person’s journey is different. Yet, these coping mechanisms can make a difference. They offer a sense of control. Support from loved ones plays a vital role too.
Preventative Measures For At-risk Diabetic Patients
Patients with diabetes face a higher risk of developing adhesive capsulitis, commonly known as frozen shoulder. Understanding preventative measures is crucial for managing this risk. Simple strategies can help maintain shoulder mobility and overall health.
Early Intervention Techniques
Early intervention is key to preventing adhesive capsulitis. Here are some effective techniques:
- Regular Stretching: Gentle stretching of the shoulder can improve flexibility.
- Range of Motion Exercises: Simple movements help keep the shoulder active.
- Physical Therapy: Working with a therapist can provide personalized exercises.
- Monitoring Blood Sugar Levels: Keeping blood sugar stable can reduce risk.
These techniques can help prevent stiffness and pain. Encourage patients to stay active and engaged in their health. Regular check-ups can also catch issues early.
Educational Programs For Prevention
Education plays a vital role in prevention. Informing patients about their risks is essential. Here are some effective educational strategies:
| Program Type | Description |
|---|---|
| Workshops | Hands-on sessions focusing on shoulder health. |
| Online Resources | Websites and videos explaining exercises and risks. |
| Community Support Groups | Sharing experiences and strategies among patients. |
Encouraging participation in these programs can raise awareness. Patients need to understand their condition. Knowledge empowers them to take charge of their health.
Emerging Therapies In Treatment
Adhesive capsulitis, often linked with diabetes, can be hard to treat. New therapies show promise in improving patient outcomes. Understanding these emerging treatments helps those affected find relief.
Innovative Medications
Recent studies highlight new medications that may help manage adhesive capsulitis. These drugs aim to reduce inflammation and pain. Here are some notable options:
- Glucocorticoids: These steroids reduce inflammation effectively.
- Hyaluronic Acid: This can improve joint lubrication and movement.
- Biologics: Target specific parts of the immune system.
These medications can be used alone or combined with other therapies. Early intervention often leads to better results.
Technological Advancements In Care
Technology plays a big role in treating adhesive capsulitis. New devices and methods are enhancing patient care:
| Technology | Benefits |
|---|---|
| Ultrasound-Guided Injections | Increased accuracy in delivering medications. |
| Telehealth Services | Convenient access to specialists from home. |
| Wearable Devices | Monitoring progress and managing pain levels. |
These advancements help tailor treatment plans. Patients can receive personalized care that fits their needs.
Nutritional Considerations And Joint Health
Adhesive capsulitis, often linked with diabetes, affects joint mobility. Nutrition plays a vital role in joint health. Proper food choices can help reduce inflammation and support overall wellness. Understanding how diet impacts this condition is essential for managing symptoms.
Dietary Recommendations
Eating a balanced diet helps manage adhesive capsulitis. Focus on foods that fight inflammation. Here are some key dietary recommendations:
- Fruits and Vegetables: Aim for colorful options. Berries, spinach, and broccoli are excellent choices.
- Whole Grains: Choose whole grains over refined grains. Oats, brown rice, and quinoa are nutritious.
- Lean Proteins: Incorporate fish, chicken, and legumes. These support muscle and joint health.
- Healthy Fats: Include sources like olive oil and avocados. They can reduce inflammation.
Stay hydrated. Drink plenty of water throughout the day. Limit sugary drinks and high-calorie snacks. Control blood sugar levels through mindful eating.
Supplements And Their Efficacy
Supplements can support joint health, especially for those with diabetes. Consider these options:
| Supplement | Benefits | Considerations |
|---|---|---|
| Omega-3 Fatty Acids | Reduces inflammation and supports joint function. | Consult a doctor before starting. |
| Glucosamine | May help repair cartilage and improve mobility. | Results can vary from person to person. |
| Vitamin D | Supports bone health and immune function. | Get levels checked before supplementing. |
Always consult with a healthcare provider. They can suggest appropriate dosages and monitor your health. Dietary changes and supplements can work together. Focus on a holistic approach to manage adhesive capsulitis and diabetes.
The Role Of Exercise In Managing Symptoms
Adhesive capsulitis, commonly known as frozen shoulder, can be painful. Those with diabetes often face a higher risk. Managing symptoms is crucial for comfort and mobility. Exercise plays a vital role in this management. Regular physical activity can help reduce pain, improve range of motion, and enhance overall function.
Effective Exercise Regimens
Choosing the right exercises is key for those with adhesive capsulitis and diabetes. Here are some effective options:
- Stretching exercises: Focus on shoulder flexibility.
- Strengthening exercises: Build muscle around the shoulder joint.
- Aerobic exercises: Boost overall fitness and help manage blood sugar.
Sample stretching exercises include:
- Cross-body arm stretch
- Overhead stretch
- Doorway stretch
Incorporating these exercises into a daily routine can lead to better outcomes.
Limitations And Precautions
Exercise is beneficial, but it comes with limitations. Here are some important precautions:
- Consult a healthcare provider before starting any exercise.
- Avoid high-impact exercises that may cause further injury.
- Listen to your body. Stop if you feel pain.
Monitoring blood sugar levels is essential during exercise. Keep snacks nearby in case of low blood sugar. Always warm up before starting exercises. Stretching helps prepare muscles and joints.
Remember, consistency is key. Regular exercise can lead to gradual improvement in symptoms.
Case Studies: Diabetic Patients With Frozen Shoulder
Understanding the link between adhesive capsulitis and diabetes is important. Case studies show that diabetic patients often face frozen shoulder. This condition limits shoulder movement and causes pain. Research highlights the need to study this relationship closely.
Clinical Progression
In diabetic patients, frozen shoulder often develops in stages:
- Stage 1: Freezing – Pain starts. Movement becomes limited.
- Stage 2: Frozen – Pain may lessen, but stiffness increases.
- Stage 3: Thawing – Gradual improvement in movement occurs.
Studies show that patients with diabetes progress through these stages differently. They often experience longer freezing and thawing phases. Increased blood sugar levels may affect healing. This leads to prolonged discomfort.
Outcomes After Intervention
Interventions for frozen shoulder in diabetic patients include:
- Physical therapy
- Medication for pain relief
- Injections of corticosteroids
Research shows positive outcomes:
| Intervention | Success Rate |
|---|---|
| Physical Therapy | 70% |
| Corticosteroid Injections | 65% |
| Medication | 60% |
Patients report reduced pain and improved movement. Early intervention is key. It can lead to better outcomes and faster recovery. Understanding the link between diabetes and frozen shoulder helps in managing both conditions.
Insurance And Cost Considerations For Treatment
Understanding the costs associated with adhesive capsulitis treatment is crucial. This condition can significantly affect individuals with diabetes. Insurance coverage varies widely. Knowing what your policy covers can ease financial stress.
Coverage For Diabetic Care
Insurance often covers treatments related to diabetes. This may include:
- Doctor visits
- Physical therapy
- Medications
- Diagnostic tests
However, specific coverage for adhesive capsulitis may differ. Here are some common insurance types:
| Insurance Type | Coverage Details |
|---|---|
| Private Insurance | May cover a variety of treatments. Check your policy. |
| Medicare | Generally covers essential services for diabetes. |
| Medicaid | Varies by state. Often covers necessary treatments. |
Review your plan carefully. Confirm coverage for any specific treatments you may need. Some procedures may require prior authorization.
Financial Burden Of Adhesive Capsulitis
The costs of adhesive capsulitis treatment can add up. Here are some common expenses:
- Doctor’s consultations
- Physical therapy sessions
- Medications for pain relief
- Imaging tests, such as MRIs
Without insurance, these costs can be overwhelming. Consider these points:
- Check if your insurance covers physical therapy.
- Ask about payment plans for high-cost treatments.
- Look for community resources that offer assistance.
Understanding these costs helps you prepare. Budgeting for treatment can ease financial stress. Consult with your healthcare provider about all available options.
Advancements In Diagnostic Procedures
Diagnosing adhesive capsulitis, also known as frozen shoulder, has improved. This is important for those with diabetes. Better diagnostic methods help doctors find the condition early. Early diagnosis leads to better treatment plans. Patients can manage their symptoms more effectively.
Accuracy Of Modern Techniques
Modern diagnostic techniques offer high accuracy. Here are some methods used:
- Ultrasound: This technique uses sound waves to create images of the shoulder. It helps identify inflammation and fluid build-up.
- Magnetic Resonance Imaging (MRI): MRI provides detailed images of shoulder structures. It shows changes in the joint capsule.
- X-rays: These help rule out other conditions. They show bone structure and any potential damage.
These methods help doctors understand the severity of the condition. They can determine if the patient has adhesive capsulitis related to diabetes.
Early Detection Benefits
Finding adhesive capsulitis early is crucial. Here are some key benefits:
- Timely Treatment: Early detection allows for prompt treatment options.
- Better Outcomes: Patients often experience quicker recovery.
- Reduced Pain: Early intervention can minimize pain levels.
- Improved Mobility: Patients can maintain better shoulder function.
With early detection, doctors can tailor treatments. This leads to a more personalized approach. Patients with diabetes can manage their overall health better. They can prevent complications from adhesive capsulitis.
Psychosocial Support Systems For Affected Individuals
Adhesive capsulitis, also known as frozen shoulder, is common in people with diabetes. Managing this condition requires more than just medical treatment. Psychosocial support systems play a vital role. They help individuals cope emotionally and socially. Support from others can ease feelings of isolation and stress.
Role Of Support Groups
Support groups offer a safe space. People share their experiences and feelings. This can reduce feelings of loneliness.
- Members share coping strategies.
- Encouragement from peers boosts morale.
- Sharing personal stories fosters understanding.
Many support groups focus on diabetes and related conditions. They provide resources and knowledge. This can help individuals manage both diabetes and adhesive capsulitis.
Mental Health Services
Mental health services are crucial for those affected. Professional help can address emotional issues. These may include anxiety or depression related to chronic pain.
- Therapists can provide coping techniques.
- Cognitive-behavioral therapy helps change negative thoughts.
- Medication may be recommended for mood disorders.
Having access to mental health support can lead to better outcomes. It allows individuals to focus on recovery. Better mental health supports physical healing.

Credit: www.sciencedirect.com
Future Directions In Research
Research on the link between Adhesive Capsulitis and Diabetes is still growing. Scientists aim to understand this connection better. New studies may lead to better treatments and prevention methods. Future research can focus on the causes, symptoms, and effective therapies.
Potential For New Discoveries
Several areas in this research hold promise. Scientists may explore new pathways. Here are some potential areas for discovery:
- Genetic Factors: Understanding genetic links can help identify at-risk individuals.
- Inflammatory Responses: Studying how inflammation affects both conditions can reveal important insights.
- Metabolic Impact: Examining how diabetes alters shoulder function may lead to new treatments.
- Physical Therapy Techniques: New methods may improve recovery for patients with both conditions.
Areas Needing Further Investigation
Researchers must address several gaps in knowledge. Important areas include:
- Prevalence Rates: More data is needed on how common Adhesive Capsulitis is in diabetes patients.
- Long-term Outcomes: Studies should track recovery over time for better understanding.
- Intervention Studies: Research must test various treatment approaches to find what works best.
- Patient Education: Understanding how to educate patients about their risks is crucial.
With these investigations, the medical community can gain valuable insights. This may lead to improved care for those affected by both Adhesive Capsulitis and Diabetes.
Frequently Asked Questions
What Is Adhesive Capsulitis?
Adhesive capsulitis, also known as frozen shoulder, causes pain and stiffness in the shoulder joint.
How Does Diabetes Affect Adhesive Capsulitis?
Diabetes increases the risk of developing adhesive capsulitis due to changes in connective tissue.
Who Is At Risk For Adhesive Capsulitis?
People with diabetes, especially type 1 and type 2, are at higher risk.
What Are The Symptoms Of Adhesive Capsulitis?
Common symptoms include shoulder pain, stiffness, and limited range of motion.
Can Adhesive Capsulitis Be Treated?
Yes, treatments include physical therapy, medication, and sometimes surgery.
How Long Does Adhesive Capsulitis Last?
Adhesive capsulitis can last from several months to a few years.
Is Adhesive Capsulitis Common In Diabetics?
Yes, studies show a significant link between diabetes and adhesive capsulitis.
What Can Diabetics Do To Prevent Adhesive Capsulitis?
Regular shoulder exercises and good diabetes management may help prevent it.
Can Adhesive Capsulitis Heal On Its Own?
Yes, some people experience improvement without treatment, but it may take time.
Should I See A Doctor For Shoulder Pain?
Yes, consult a doctor if you have persistent shoulder pain or stiffness.
Conclusion
Adhesive capsulitis, or frozen shoulder, affects many people with diabetes. This condition can cause pain and limit movement. Understanding this link is important for better management. Early diagnosis and treatment can help reduce symptoms. Regular exercise and physical therapy also play a key role.
Managing blood sugar levels may improve shoulder health. Stay informed about your health. Consult with a healthcare provider for personalized advice. Awareness can lead to better outcomes. Take steps today to protect your shoulder and overall well-being.


