Diabetes Mellitus Posterior Capsule Opacification (DMPCO) is a condition that can affect people with diabetes. It involves the clouding of the capsule behind the eye lens, leading to vision problems.
Understanding DMPCO is crucial for those living with diabetes. This condition can develop after cataract surgery, especially in diabetic patients. Symptoms may include blurry vision and difficulty seeing in bright light. The risk increases as diabetes can affect eye health over time.
Awareness and early detection are key. Regular eye check-ups help catch issues early. This blog post will explore the causes, symptoms, and treatment options for DMPCO. With this knowledge, patients can take steps to protect their vision and overall eye health.

Credit: www.researchgate.net
Introduction To Diabetes And Eye Health
Diabetes affects many parts of the body. One area that suffers is eye health. High blood sugar can lead to serious eye conditions. These conditions can cause vision loss. Understanding diabetes and its impact on the eyes is important.
Link Between Diabetes Mellitus And Eye Conditions
Diabetes Mellitus can lead to several eye problems. Here are some key points:
- Diabetic Retinopathy: Damage to the retina from high blood sugar.
- Cataracts: Clouding of the lens in the eye, leading to blurry vision.
- Glaucoma: Increased pressure in the eye, which can harm the optic nerve.
These conditions can worsen over time. Regular eye exams help catch problems early.
Overview Of Posterior Capsule Opacification (pco)
Posterior Capsule Opacification (PCO) is a common issue after cataract surgery. It occurs when the back of the lens capsule becomes cloudy. This can affect vision. Here are some important facts:
| Aspect | Description |
|---|---|
| Cause | Natural healing process after cataract surgery. |
| Symptoms | Blurry vision, glare, and difficulty seeing at night. |
| Treatment | YAG laser capsulotomy is a common procedure. |
PCO can develop months or years after surgery. Awareness and timely treatment can restore clear vision.
Understanding Posterior Capsule Opacification
Posterior Capsule Opacification (PCO) is a common condition. It can happen after cataract surgery. This condition affects vision. Understanding PCO helps in managing it better.
What Is Pco?
PCO occurs when the capsule behind the lens becomes cloudy. This capsule holds the lens in place. After cataract surgery, the capsule can thicken. This thickening leads to blurry vision. PCO is sometimes called secondary cataract.
- PCO affects many patients post-surgery.
- It can develop months or years later.
- Symptoms include blurred vision and glare.
The Process Of Capsular Haze Development
Capsular haze develops due to cell growth. After surgery, some lens cells remain. These cells can multiply over time. They cause the capsule to become cloudy.
Factors that contribute to PCO:
- Type of cataract surgery.
- Age of the patient.
- Underlying health issues, like diabetes.
The process can be broken down into stages:
- Initial Cell Growth: Cells start to multiply.
- Cloudiness Formation: Cells create a haze.
- Visual Symptoms: Vision becomes blurry.
Recognizing PCO early is key. Regular check-ups help spot changes. Treatment is effective and usually simple.
Diabetes As A Risk Factor For Pco
Diabetes is a major health concern worldwide. One of its complications is the risk of Posterior Capsule Opacification (PCO). PCO can occur after cataract surgery. Understanding the link between diabetes and PCO is essential for better eye health. Let’s explore how diabetes increases the risk of developing PCO.
How Diabetes Contributes To Pco Risk
Diabetes affects the body in many ways. It can lead to changes in the lens of the eye. These changes can increase the chances of PCO. Here are some key factors:
- High Blood Sugar Levels: Elevated glucose can cause lens swelling.
- Inflammation: Diabetes may cause chronic inflammation in the body.
- Oxidative Stress: High sugar levels lead to oxidative damage.
- Age-Related Factors: Older diabetic patients have a higher risk.
These factors contribute to the development of PCO after cataract surgery.
Statistical Relationship Between Diabetes And Pco
Research shows a strong link between diabetes and PCO. The statistics are significant:
| Study | Diabetic Patients with PCO (%) | Non-Diabetic Patients with PCO (%) |
|---|---|---|
| Study A | 30% | 10% |
| Study B | 25% | 8% |
| Study C | 35% | 12% |
These studies show that diabetes increases PCO risk significantly. Diabetic patients are three times more likely to develop PCO.
Awareness is crucial for diabetic individuals. Regular eye check-ups can help manage risks. Early detection can lead to better outcomes.
Symptoms Of Pco In Diabetic Patients
Diabetes can lead to various eye problems, including Posterior Capsule Opacification (PCO). PCO occurs when the lens capsule becomes cloudy. This can cause vision issues for diabetic patients. Recognizing the symptoms early is crucial for effective treatment.
Common Signs Of Pco
PCO symptoms can vary among individuals. Here are some common signs to watch for:
- Blurry Vision: Vision may become unclear or fuzzy.
- Glare and Halos: Bright lights can create glare or halos.
- Difficulty Seeing at Night: Night vision can become challenging.
- Frequent Changes in Prescription: Regular updates to glasses or contact lenses may be needed.
- Double Vision: Seeing two images instead of one can occur.
These symptoms may develop gradually. Regular eye exams are important for monitoring changes.
Distinguishing Pco From Diabetic Retinopathy
It is important to differentiate PCO from diabetic retinopathy. Both conditions affect vision but have different causes and treatments. Here’s how to tell them apart:
| Feature | PCO | Diabetic Retinopathy |
|---|---|---|
| Cause | Clouding of the lens capsule | Damage to retinal blood vessels |
| Symptoms | Blurry vision, glare, halos | Dark spots, floating shapes, vision loss |
| Treatment | YAG laser capsulotomy | Laser therapy, medications |
Understanding these differences helps in seeking the right treatment. Regular check-ups can help identify these symptoms early.
Diagnosis Of Pco In Diabetes
Diabetes can lead to a condition called Posterior Capsule Opacification (PCO). PCO occurs after cataract surgery. It causes blurred vision and discomfort. Diagnosing PCO in diabetics can be complex. Early detection is essential for effective treatment. Understanding the diagnostic procedures helps in managing this condition.
Diagnostic Procedures For Pco
Doctors use various methods to diagnose PCO. These procedures help in identifying the condition accurately. Common diagnostic procedures include:
- Visual Acuity Test: Measures how well a patient can see.
- Slit-Lamp Examination: Provides a detailed view of the eye.
- OCT (Optical Coherence Tomography): Creates cross-sectional images of the eye.
- Ultrasound Biomicroscopy: Uses sound waves to view eye structures.
These tests allow the doctor to assess the clarity of the lens. They help determine if PCO is present.
Challenges In Diagnosing Pco In Diabetics
Diagnosing PCO in diabetic patients poses unique challenges. Some of these challenges include:
- Changes in Eye Structure: Diabetes can alter the eye’s anatomy.
- Comorbid Conditions: Other eye diseases may complicate diagnosis.
- Difficulty in Assessing Symptoms: Diabetics may have other vision issues.
These factors make it harder to identify PCO early. Regular eye exams are vital for diabetics. They help catch PCO before it worsens.
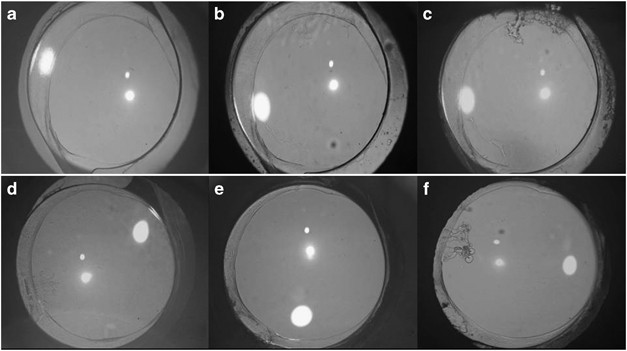
Credit: www.nature.com
Surgical Treatment Options For Pco
Diabetes Mellitus can lead to complications like Posterior Capsule Opacification (PCO). PCO can cause blurry vision after cataract surgery. Surgical treatment options are available to improve vision. Let’s explore two main surgical options for treating PCO.
Nd:yag Laser Capsulotomy
Nd:YAG laser capsulotomy is a common procedure for PCO. This treatment uses a laser to create an opening in the cloudy capsule behind the lens.
- The procedure is quick, often taking less than 10 minutes.
- It is performed in an outpatient setting.
- Patients usually feel little to no pain.
- Vision improvement can be noticed almost immediately.
After the procedure, the doctor may recommend follow-up visits. These visits help ensure the eye heals properly. Most patients return to normal activities quickly.
Risks Of Surgery For Diabetic Patients
Surgery carries some risks, especially for diabetic patients. Understanding these risks is important before proceeding.
| Risk | Description |
|---|---|
| Infection | Risk of infection increases after any surgery. |
| Bleeding | Diabetes can lead to increased bleeding during surgery. |
| Retinal Issues | Diabetics may face retinal problems post-surgery. |
| Delayed Healing | Wound healing may take longer in diabetic patients. |
Discuss these risks with your doctor. They can help you understand how diabetes affects surgery outcomes. Knowing the risks can aid in making informed decisions.
Non-surgical Management Of Pco In Diabetes
Managing Posterior Capsule Opacification (PCO) in diabetic patients requires careful consideration. Non-surgical options can help control symptoms. These methods focus on medications, eye drops, and lifestyle changes. They aim to improve vision and comfort without surgery.
Medications And Eye Drops
Specific medications and eye drops can help manage PCO symptoms. These treatments focus on reducing inflammation and improving eye health. Common options include:
- Anti-inflammatory eye drops: These help reduce swelling.
- Artificial tears: These relieve dryness and irritation.
- Medicated drops: These can help with pressure in the eye.
Always follow your eye doctor’s advice when using these treatments. Regular check-ups are essential to monitor eye health.
Lifestyle Adjustments For Managing Symptoms
Making lifestyle changes can also help manage PCO symptoms effectively. Consider these adjustments:
- Diet: Eat a balanced diet rich in fruits and vegetables.
- Hydration: Drink plenty of water to keep your eyes moist.
- Regular exercise: Exercise improves blood circulation and overall health.
- Avoid smoking: Smoking can worsen eye conditions.
- Manage diabetes: Keep blood sugar levels stable to reduce eye complications.
Simple changes can have a significant impact on your eye health. Stay proactive about your health for better outcomes.
Impact Of Glycemic Control On Pco Development
Glycemic control plays a key role in the development of Posterior Capsule Opacification (PCO). People with diabetes often face higher risks of eye complications. High blood sugar levels can lead to changes in the eye’s lens. These changes can cause PCO, which affects vision.
The Role Of Blood Sugar Levels In Pco
Blood sugar levels directly influence the risk of developing PCO. Here are some important points:
- High Blood Sugar: Increases the chance of PCO.
- Fluctuating Levels: Unstable blood sugar can worsen PCO risks.
- Long-term Effects: Chronic high levels can lead to permanent eye damage.
Studies show that better glycemic control can lower PCO development. Lower blood sugar reduces the lens’s cloudiness.
Controlling Diabetes To Prevent Pco
Maintaining stable blood sugar is crucial for eye health. Here are effective ways to control diabetes:
- Regular Monitoring: Check blood sugar levels often.
- Healthy Diet: Focus on low-sugar and balanced meals.
- Exercise: Engage in daily physical activity.
- Medication: Take prescribed diabetes medication as directed.
- Routine Check-ups: Visit your doctor regularly for eye exams.
Following these steps can significantly reduce the risk of PCO. Good glycemic control leads to better overall health.
Prevention Strategies For Diabetics
Preventing Diabetes Mellitus Posterior Capsule Opacification is vital for diabetics. Simple steps can help. Regular care and awareness can make a big difference.
Regular Eye Examinations
Regular eye exams are important for diabetics. They help detect problems early. Here are some key points:
- Visit an eye doctor at least once a year.
- Get a comprehensive eye exam.
- Ask about tests for diabetic eye diseases.
- Report any changes in vision immediately.
Early detection can prevent serious issues. Eye health impacts overall health.
Importance Of Maintaining Optimal Blood Glucose
Keeping blood glucose levels stable is crucial. High levels can lead to complications. Here are some tips:
- Monitor blood sugar regularly.
- Follow a balanced diet.
- Exercise regularly.
- Take medications as prescribed.
Stable blood sugar levels can reduce risks. Focus on healthy habits. Small changes can lead to big improvements.
Talk to your doctor about managing your diabetes. Good control helps protect your vision.
Complications Associated With Pco In Diabetic Patients
Diabetes can lead to many eye problems. One serious issue is Posterior Capsule Opacification (PCO). This condition occurs when the lens capsule becomes cloudy after cataract surgery. Diabetic patients often face a higher risk of complications from PCO. Understanding these complications is important for better management.
Potential For Increased Pco Recurrence
Diabetic patients may experience increased recurrence of PCO. Here are some reasons why:
- Diabetes affects the healing process.
- High blood sugar levels can lead to inflammation.
- Changes in lens capsule structure may occur.
Studies show that diabetic patients have a higher chance of needing repeat treatments for PCO. This can lead to more surgeries and longer recovery times. Regular eye exams are crucial for early detection.
Managing Complications Post-surgery
Managing complications after surgery is vital for diabetic patients. Follow these steps:
- Monitor blood sugar levels closely.
- Attend all follow-up appointments.
- Report any vision changes immediately.
Common post-surgery complications include:
| Complication | Symptoms |
|---|---|
| Infection | Redness, swelling, pain |
| Inflammation | Blurred vision, sensitivity to light |
| Retinal Detachment | Flashes of light, sudden vision loss |
Timely management can prevent severe issues. Consult an eye doctor if complications arise. Early treatment leads to better outcomes.
Cataract Surgery In Diabetic Patients
Cataract surgery is common for diabetic patients. Diabetes can cause vision problems. This surgery helps improve sight. But it also has risks, like Posterior Capsule Opacification (PCO). Understanding these risks is important for better eye health.
How Cataract Surgery Can Lead To Pco
Cataract surgery removes the cloudy lens. It replaces it with a clear artificial lens. In some cases, the membrane behind the lens can become cloudy. This condition is called Posterior Capsule Opacification (PCO).
Diabetic patients are at a higher risk for PCO. Factors include:
- Duration of diabetes
- Control of blood sugar levels
- Previous eye surgeries
Symptoms of PCO can include:
- Blurry vision
- Increased sensitivity to light
- Glare around lights
If you experience these symptoms after surgery, consult your eye doctor. They may recommend a simple outpatient procedure to clear the cloudiness.
Precautions And Care Post-cataract Surgery
Proper care after cataract surgery is crucial. Follow these precautions:
- Use prescribed eye drops regularly.
- Avoid touching or rubbing your eyes.
- Wear sunglasses outdoors to protect your eyes.
- Limit activities like bending or heavy lifting.
Regular check-ups are essential. Your doctor will monitor your recovery and check for PCO. Maintain healthy blood sugar levels. This can help reduce complications.
Proper care ensures the best outcome after cataract surgery. Stay informed and proactive about your eye health.
Credit: clinicaloptometry.scholasticahq.com
Nutritional Considerations For Eye Health
Good nutrition plays a key role in maintaining eye health. For people with diabetes, managing blood sugar levels is vital. Proper dietary choices can help reduce the risk of Posterior Capsule Opacification (PCO). Here are some essential aspects to consider.
Dietary Choices To Reduce Pco Risk
Making smart food choices can lower the risk of PCO. Focus on foods that support eye health and control blood sugar. Here are some tips:
- Eat whole grains: Brown rice, quinoa, and oats help maintain stable blood sugar levels.
- Include leafy greens: Spinach, kale, and broccoli are rich in antioxidants.
- Choose healthy fats: Avocados, nuts, and olive oil support overall health.
- Limit sugar intake: Reduce sugary snacks and beverages to control blood sugar.
- Stay hydrated: Drink plenty of water to support eye function.
Vitamins And Supplements For Eye Health
Certain vitamins and supplements can aid eye health. They may help prevent PCO and other issues. Consider these:
| Vitamin/Supplement | Benefits |
|---|---|
| Vitamin A | Supports night vision and overall eye health. |
| Vitamin C | Helps protect against cataracts and supports blood vessels. |
| Vitamin E | Acts as an antioxidant to protect eye cells. |
| Omega-3 Fatty Acids | Supports retinal health and may reduce dry eyes. |
| Lutein and Zeaxanthin | Helps filter harmful blue light and protects the retina. |
Consult a healthcare professional before taking any supplements. They can provide personalized advice based on individual health needs.
Innovative Research On Pco And Diabetes
Recent studies highlight the link between Diabetes Mellitus and Posterior Capsule Opacification (PCO). Researchers focus on improving treatment methods. Their goal is to help patients with diabetes manage PCO effectively. This section explores recent findings and future directions in PCO management.
Recent Advances In Pco Treatment
Researchers have made significant strides in PCO treatment for diabetics. Here are some key advances:
- Use of laser surgery to remove cloudy lenses.
- Development of medications to prevent PCO formation.
- Enhanced screening methods for early detection.
Laser surgery has become a common method. It helps clear vision quickly. Medications show promise in reducing PCO risk. Early screening can identify PCO sooner, leading to better outcomes.
Future Of Pco Management For Diabetics
The future of PCO management looks bright. Ongoing research aims to achieve the following:
- Personalized treatments based on patient profiles.
- Improved educational programs for patients.
- Collaboration between ophthalmologists and endocrinologists.
Personalized treatments could lead to better care. Education helps patients understand their risks. Collaboration ensures comprehensive management of diabetes and PCO.
| Research Focus | Expected Outcome |
|---|---|
| Laser Technologies | Faster recovery times |
| Medication Development | Reduced PCO incidence |
| Patient Education | Higher awareness and compliance |
The Role Of Ophthalmologists And Diabetologists
Ophthalmologists and diabetologists play a key role in managing Diabetes Mellitus Posterior Capsule Opacification. Their teamwork is vital for patient care. Both specialists focus on different aspects of diabetes. Together, they provide comprehensive treatment for patients.
Collaborative Care Approach
A collaborative care approach is essential for effective treatment. Ophthalmologists diagnose and treat eye conditions. Diabetologists manage diabetes and its complications. This partnership improves patient outcomes.
- Regular eye exams are crucial for early detection.
- Monitoring blood sugar levels helps prevent complications.
- Shared patient records ensure everyone is informed.
Both specialists educate patients about their conditions. They discuss the importance of keeping blood sugar levels stable. They also highlight the need for routine eye check-ups.
Referral And Treatment Coordination
Referral between ophthalmologists and diabetologists is important. Early referrals can help prevent serious eye issues. Patients should see both specialists regularly. This ensures all aspects of diabetes are managed.
| Specialist | Focus Area | Patient Actions |
|---|---|---|
| Ophthalmologist | Eye health and vision | Schedule regular eye exams |
| Diabetologist | Diabetes management | Monitor blood sugar levels |
Coordination of treatment plans helps avoid complications. Both specialists discuss treatment options. They ensure that patients understand their roles in managing their health. This teamwork creates a supportive environment for better health.
Patient Education And Self-care
Understanding diabetes and its effects on eye health is essential. Patient education plays a key role. It helps in managing Diabetes Mellitus Posterior Capsule Opacification (PCO). Knowledge empowers patients to take charge of their health. Self-care practices can prevent complications and improve overall well-being.
Importance Of Patient Awareness
Awareness is the first step in effective management of PCO. Patients need to know how diabetes affects vision. Here are some crucial points to consider:
- Know the symptoms of PCO: blurred vision, glare, and halos.
- Understand the link between diabetes and eye conditions.
- Recognize the importance of regular eye check-ups.
Patients who are informed make better decisions about their health. They can spot issues early. Early detection is vital to prevent further complications.
Self-monitoring Techniques For Eye Health
Self-monitoring is a powerful tool for managing eye health. Here are some techniques patients can use:
- Regular Eye Exams: Schedule eye exams at least once a year.
- Vision Tests: Use simple vision tests at home.
- Report Changes: Notify your doctor of any vision changes.
- Control Blood Sugar Levels: Keep blood sugar within target ranges.
Tracking your eye health can prevent serious issues. Use a notebook or an app to record changes. This information helps your doctor provide better care.
| Self-Monitoring Technique | Frequency | Notes |
|---|---|---|
| Eye Exams | Once a year | Essential for early detection |
| Vision Tests | Monthly | Simple tests can be done at home |
| Blood Sugar Monitoring | Daily | Maintain levels within target |
These self-care practices support better eye health. Empowerment through knowledge leads to better outcomes. Stay informed, stay healthy.
Technology’s Role In Managing Pco
Technology plays a vital role in managing Posterior Capsule Opacification (PCO). New tools help doctors diagnose and treat this condition effectively. Patients benefit from improved monitoring and care. Here’s how technology is changing the landscape of PCO management.
Advancements In Diagnostic Tools
Modern diagnostic tools make identifying PCO easier. These tools include:
- OCT (Optical Coherence Tomography): Offers detailed images of the eye.
- Ultrasound Biomicroscopy: Provides high-resolution images of the eye’s structures.
- Slit-Lamp Examination: Allows doctors to see the eye in detail.
These advancements lead to faster and more accurate diagnosis. Early detection can prevent vision loss. Patients receive timely treatment, improving their quality of life.
Telemedicine And Remote Monitoring
Telemedicine is changing how patients manage PCO. Patients can consult specialists without traveling. This saves time and reduces stress. Remote monitoring tools allow for:
- Regular check-ups using video calls.
- Tracking symptoms through mobile apps.
- Receiving immediate advice from healthcare providers.
Remote tools help in managing PCO symptoms effectively. Patients feel more connected to their healthcare team. This approach leads to better outcomes and patient satisfaction.
Insurance And Cost Considerations
Understanding the costs of treating Diabetes Mellitus Posterior Capsule Opacification (PCO) is essential. Medical treatment can be expensive. Insurance can help offset some of these costs. Knowing what your insurance covers is important for planning treatment.
Covering The Cost Of Pco Treatment
Costs for PCO treatment can vary. Factors include:
- Type of treatment needed
- Location of the procedure
- Surgeon’s fees
- Facility charges
Here is a basic outline of potential costs:
| Treatment Type | Estimated Cost |
|---|---|
| YAG Laser Capsulotomy | $1,500 – $3,000 |
| Follow-up Visits | $100 – $300 |
| Medications | $20 – $200 |
Check if your insurance plan covers these costs. Contact your insurance provider for details on your specific plan. Some plans may require pre-approval. Others may have a deductible or co-payment. Always confirm before scheduling your treatment.
Financial Assistance And Resources
Many resources are available to help with costs. Consider the following options:
- Nonprofit organizations
- Government programs
- Hospital financial aid
Here are some resources you can explore:
- American Diabetes Association: They offer resources for financial support.
- State Medicaid Programs: Check if you qualify for assistance.
- Local charities: Many provide support for medical costs.
Research these options. Apply for assistance if needed. Every bit helps in managing the costs of PCO treatment.
Case Studies: Pco Management In Diabetics
Posterior capsule opacification (PCO) is common in diabetic patients. Managing PCO in these individuals requires careful attention. Here, we explore real case studies. These narratives highlight successful treatments and lessons learned from complex cases.
Successful Treatment Narratives
Several patients with diabetes underwent treatment for PCO. Their stories show how effective management can be.
| Patient | Age | Treatment | Outcome |
|---|---|---|---|
| Patient A | 65 | YAG Laser Capsulotomy | Vision improved from 20/200 to 20/40 |
| Patient B | 72 | Phacoemulsification | Significant vision restoration |
| Patient C | 58 | YAG Laser Capsulotomy | Stable vision at 20/30 |
These cases show that timely intervention yields positive results. The use of YAG laser capsulotomy is prevalent. Patients experience quick recovery and improved vision.
Lessons Learned From Complex Cases
Not all PCO cases in diabetics are straightforward. Some patients face complications. Analyzing these cases reveals key insights.
- Patient D had uncontrolled diabetes.
- Post-treatment, they experienced delayed healing.
- Regular monitoring became essential.
Another case involved Patient E. They had a history of glaucoma.
- PCO treatment was challenging.
- Collaboration with a glaucoma specialist was necessary.
- Multidisciplinary care led to a better outcome.
These complex cases emphasize the need for personalized treatment plans. Understanding each patient’s history is crucial. This approach ensures better management of PCO in diabetic patients.
Support Systems And Resources
Dealing with Diabetes Mellitus Posterior Capsule Opacification can be tough. Support systems and resources can help patients and caregivers manage their health better. These systems provide emotional support, education, and practical advice. Connecting with others facing similar challenges makes a difference.
Support Groups And Counseling
Support groups offer a safe space. Patients and caregivers can share their experiences. Here are some benefits of joining a support group:
- Meet others who understand your journey.
- Share feelings and reduce loneliness.
- Gain practical tips for daily life.
- Learn coping strategies from others.
Counseling also plays a key role. A trained counselor can help with emotional struggles. They can guide patients through feelings of anxiety or depression. Seeking professional help is a sign of strength, not weakness.
Educational Material For Patients And Caregivers
Knowledge is power. Access to educational materials helps patients and caregivers understand their condition. Here are some resources to consider:
| Resource Type | Description |
|---|---|
| Brochures | Provide basic information on symptoms and treatments. |
| Websites | Offer articles, videos, and forums for support. |
| Workshops | Conduct hands-on learning about diabetes management. |
| Books | Cover personal stories and expert advice. |
Utilizing these resources can enhance understanding. This knowledge helps in making informed choices. Staying informed encourages better health management. Seek out these materials regularly.
Conclusion: Living With Pco And Diabetes
Living with Posterior Capsule Opacification (PCO) can be challenging. For those with Diabetes Mellitus, the journey can be even more complex. Understanding this condition helps in managing it better. Here’s how to adapt and what the future may hold.
Adapting To The New Normal
Adjusting to life with PCO and diabetes involves several strategies:
- Regular eye check-ups are crucial.
- Maintain stable blood sugar levels.
- Follow a healthy diet rich in nutrients.
- Stay active with regular exercise.
- Seek support from healthcare professionals.
Daily routines may need changes. Simple tasks can become harder. It is important to:
- Use adaptive devices for easier vision.
- Take breaks during activities that require focus.
- Communicate with family and friends about your needs.
Continued Research And Hope For The Future
Research on PCO and diabetes is ongoing. New treatments and technologies are emerging. Here are key areas of focus:
| Research Area | Description |
|---|---|
| New Surgical Techniques | Improving outcomes for PCO patients. |
| Medical Treatments | Developing medications to manage symptoms. |
| Diabetes Management | Innovations in glucose monitoring and control. |
Hope exists for better management of these conditions. Collaboration between researchers, doctors, and patients is vital. Staying informed can empower those affected.
With the right strategies, people can live fulfilling lives. Awareness and education play key roles in overcoming challenges. Embracing a proactive approach is essential.
Frequently Asked Questions
What Is Diabetes Mellitus Posterior Capsule Opacification?
Diabetes mellitus posterior capsule opacification is a clouding of the lens capsule after cataract surgery in diabetic patients.
What Causes Posterior Capsule Opacification In Diabetes?
High blood sugar levels can lead to changes in the eye’s lens, causing opacification.
How Is Posterior Capsule Opacification Diagnosed?
It is diagnosed through a comprehensive eye exam that checks vision and lens clarity.
What Are The Symptoms Of Posterior Capsule Opacification?
Symptoms include blurry vision, glare, and difficulty seeing in low light.
Can Posterior Capsule Opacification Be Treated?
Yes, it can be treated with a simple outpatient procedure called YAG laser capsulotomy.
How Long After Cataract Surgery Does Opacification Occur?
It can occur weeks to years after cataract surgery, especially in diabetic patients.
Is Posterior Capsule Opacification Common In Diabetic Patients?
Yes, diabetic patients are at a higher risk for developing this condition.
What Is The Recovery Time After Treatment?
Recovery is usually quick, with most patients noticing improvements within a day or two.
Are There Risks Associated With Yag Laser Capsulotomy?
Risks are minimal but can include temporary eye pressure increase or retinal detachment.
How Can I Reduce The Risk Of Posterior Capsule Opacification?
Maintaining good blood sugar control and regular eye check-ups can help lower the risk.
Conclusion
Diabetes mellitus can lead to posterior capsule opacification. This condition affects vision after cataract surgery. Understanding its causes helps in prevention and treatment. Regular eye check-ups are crucial for early detection. Timely intervention can improve outcomes and restore sight. Patients should discuss any vision changes with their doctor.
Knowledge and awareness empower better management of eye health. Stay informed to protect your vision from complications. Taking action now can lead to a brighter future for your eyes.


