Adhesive capsulitis, often known as frozen shoulder, can be a painful condition. This issue is especially common among people with diabetes mellitus.
Adhesive capsulitis occurs when the shoulder becomes stiff and hard to move. It can cause significant discomfort and limit daily activities. People with diabetes are at a higher risk for developing this condition. Research shows that the connection between diabetes and adhesive capsulitis is strong.
Understanding this link is important for managing both health issues. Knowing the symptoms and treatments available can help patients find relief. This blog will explore the relationship between adhesive capsulitis and diabetes mellitus, helping you understand why this condition occurs and how to address it effectively.
Introduction To Adhesive Capsulitis
Adhesive capsulitis, commonly known as frozen shoulder, is a painful condition. It limits shoulder movement. This condition often develops slowly. It can affect daily activities and quality of life. Understanding adhesive capsulitis helps in managing symptoms effectively.
Symptoms Of Frozen Shoulder
Recognizing the symptoms of frozen shoulder is essential. Symptoms often appear in three stages:
- Freezing Stage: Gradual onset of pain and limited motion.
- Frozen Stage: Pain may decrease, but stiffness increases.
- Thawing Stage: Range of motion begins to improve.
Common symptoms include:
- Sharp pain in the shoulder.
- Difficulty reaching overhead.
- Stiffness in the shoulder joint.
- Pain that worsens at night.
Early diagnosis is important. It helps in reducing long-term complications.
Link Between Diabetes And Joint Pain
Diabetes can increase the risk of developing adhesive capsulitis. High blood sugar levels can affect connective tissues. This leads to joint pain and stiffness. Studies show that diabetics are more likely to experience frozen shoulder.
Here are some important points:
| Condition | Risk Factor |
|---|---|
| Adhesive Capsulitis | Higher in diabetic patients |
| Joint Pain | Common in uncontrolled diabetes |
Managing blood sugar levels may help reduce symptoms. Regular check-ups are important for diabetic patients.
Diabetes Mellitus Overview
Diabetes Mellitus is a serious health condition. It affects how the body uses blood sugar (glucose). Glucose is vital for energy. Understanding diabetes is crucial for managing related issues like adhesive capsulitis.
Type 1 Vs Type 2 Diabetes
Diabetes is mainly of two types:
- Type 1 Diabetes: This type occurs when the body cannot produce insulin. It often starts in childhood or young adulthood.
- Type 2 Diabetes: This type is more common. The body does not use insulin well. It usually develops in adults but can occur in children.
| Feature | Type 1 Diabetes | Type 2 Diabetes |
|---|---|---|
| Age of Onset | Usually childhood or adolescence | Usually adulthood |
| Insulin Production | Little to none | Insulin resistant |
| Treatment | Insulin therapy required | Diet, exercise, and medication |
How Diabetes Affects The Body
Diabetes can lead to various complications. High blood sugar damages blood vessels and nerves. This can cause:
- Heart disease
- Kidney damage
- Nerve damage
- Eye problems
Joint health can also suffer. Adhesive capsulitis, or frozen shoulder, is common. It limits movement and causes pain. Managing blood sugar is vital to prevent these issues.
Regular check-ups and a healthy lifestyle help. Monitor blood sugar levels. Follow a balanced diet. Stay active to reduce complications.
Frozen Shoulder: A Diabetic Complication
Frozen shoulder, also known as adhesive capsulitis, is common among diabetics. This condition limits shoulder movement and causes pain. People with diabetes face a higher risk of developing frozen shoulder. Understanding its prevalence and risk factors is important for management and prevention.
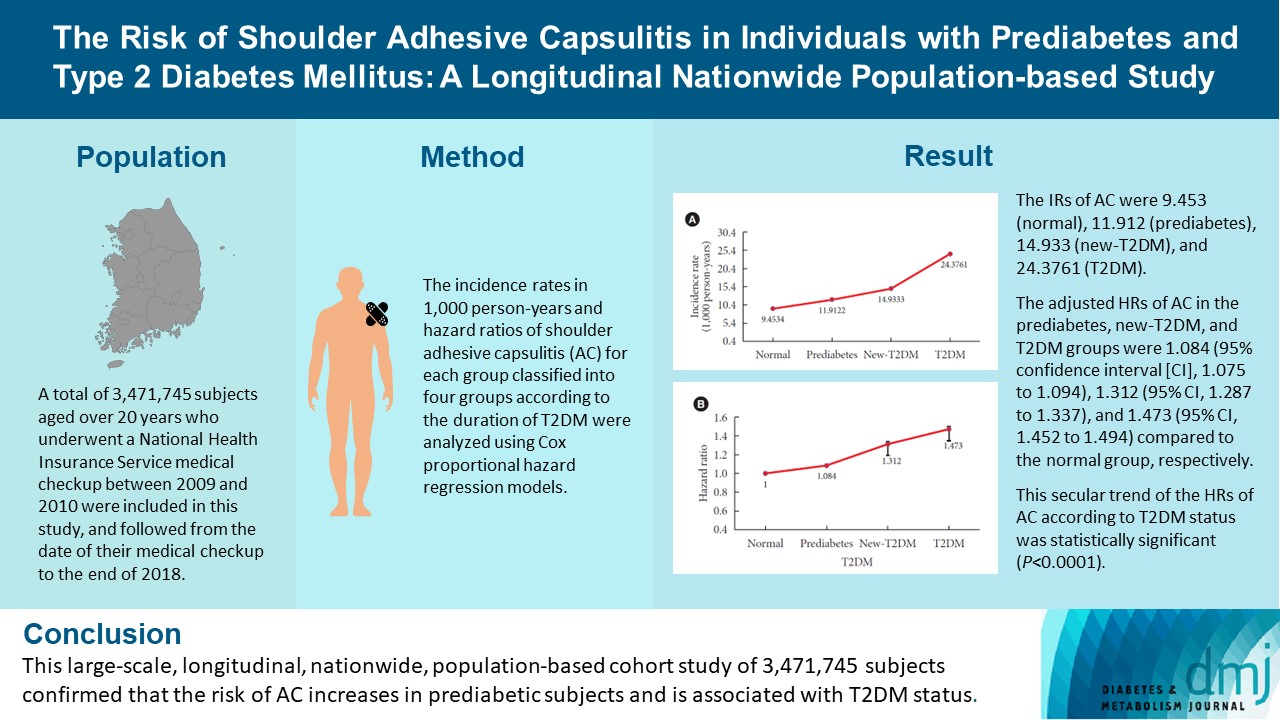
Prevalence In Diabetic Patients
Frozen shoulder is more common in people with diabetes than in the general population. Studies show that:
- Up to 20% of diabetics may develop frozen shoulder.
- The risk is higher for those with poorly controlled blood sugar.
- It typically affects people aged 40 to 60 years.
Research indicates that frozen shoulder occurs more in women. It can also appear in both Type 1 and Type 2 diabetes patients. Early diagnosis is crucial for effective treatment.
Risk Factors For Diabetics
Several factors increase the risk of frozen shoulder in diabetics:
| Risk Factor | Description |
|---|---|
| Blood Sugar Levels | High levels can lead to nerve damage. |
| Age | Risk increases with age, especially over 40. |
| Gender | Women are more likely to develop it. |
| Previous Shoulder Injuries | Past injuries can trigger frozen shoulder. |
| Other Health Issues | Conditions like thyroid disorders can increase risk. |
Identifying these risk factors can help in prevention. Regular check-ups and managing diabetes are key steps.
Early Signs Of Adhesive Capsulitis
Adhesive capsulitis, also known as frozen shoulder, often affects people with diabetes mellitus. Understanding the early signs can help in seeking timely treatment. Early identification may lead to better outcomes and relief from discomfort.
Stages Of Frozen Shoulder
| Stage | Duration | Description |
|---|---|---|
| Freezing Stage | 6-9 months | Pain increases. Limited movement begins. |
| Frozen Stage | 4-6 months | Pain may decrease. Movement is very limited. |
| Thawing Stage | 6 months to 2 years | Gradual return of motion. Pain continues to lessen. |
Recognizing Initial Symptoms
Recognizing the initial symptoms of adhesive capsulitis is vital. Common signs include:
- Shoulder pain: Often sharp or aching.
- Stiffness: Difficulty moving the shoulder.
- Decreased range of motion: Trouble reaching overhead.
- Pain at night: Discomfort can disrupt sleep.
These symptoms may start gradually. Ignoring them can lead to more severe issues. Early intervention can improve recovery.
Impact Of Blood Glucose Control
Blood glucose control plays a vital role in managing Adhesive Capsulitis. This condition, also known as frozen shoulder, often affects those with Diabetes Mellitus. Poor blood sugar levels can worsen joint health. Understanding this connection can help improve treatment outcomes.
Blood Sugar Management
Managing blood sugar is crucial for individuals with diabetes. Consistent levels can reduce complications. Here are some key points on effective blood sugar management:
- Check blood sugar regularly.
- Follow a balanced diet.
- Exercise regularly.
- Take medications as prescribed.
- Monitor stress levels.
Each of these steps contributes to overall health. Consistent management can lead to fewer episodes of frozen shoulder. Patients should aim for stable blood sugar levels.
Correlation With Joint Health
The link between blood glucose control and joint health is significant. High blood sugar can lead to inflammation. This inflammation can contribute to joint stiffness and pain.
| Blood Sugar Level | Impact on Joint Health |
|---|---|
| Below 140 mg/dL | Better joint mobility and less pain |
| 140-180 mg/dL | Moderate stiffness and discomfort |
| Above 180 mg/dL | Increased inflammation and severe pain |
Maintaining lower blood sugar levels helps reduce joint pain. Patients with better control report less discomfort in their shoulders. This connection is important for treatment strategies.
In summary, blood glucose control is essential in managing Adhesive Capsulitis. Good management leads to improved joint health. Focus on maintaining stable blood sugar levels for better outcomes.
Diagnosis Of Adhesive Capsulitis
Diagnosing Adhesive Capsulitis, commonly known as frozen shoulder, can be challenging. Doctors rely on various methods to understand the condition. Early diagnosis is crucial for effective treatment. Patients often experience limited shoulder movement and pain.
Diagnostic Tests
Several diagnostic tests help confirm Adhesive Capsulitis. These tests assess the range of motion and identify pain levels. Common tests include:
- Physical Examination: Doctors check shoulder movement.
- X-rays: These show bone structure and rule out other issues.
- MRI: This imaging test provides detailed pictures of soft tissues.
- Ultrasound: This test visualizes the shoulder joint and surrounding tissues.
These tests help determine the severity of the condition. They also guide treatment options.
Role Of Medical History
A thorough medical history plays a vital role in diagnosis. Doctors ask about:
- Previous shoulder injuries
- Existing health conditions like Diabetes Mellitus
- Family history of joint problems
- Duration and intensity of shoulder pain
Understanding these factors helps doctors make informed decisions. Knowing if a patient has Diabetes Mellitus is crucial. This condition increases the risk of Adhesive Capsulitis.
By combining medical history with diagnostic tests, doctors can accurately diagnose Adhesive Capsulitis. This approach ensures patients receive proper care.
Non-pharmaceutical Management
Managing Adhesive Capsulitis in people with Diabetes Mellitus often requires more than just medication. Non-pharmaceutical methods can help reduce pain and improve movement. This section covers effective strategies like physical therapy and lifestyle changes.
Physical Therapy Exercises
Physical therapy plays a key role in recovery. Specific exercises can help regain shoulder motion. Here are some effective exercises:
- Pendulum Stretch: Lean forward and let your arm hang down. Gently swing your arm in small circles.
- Cross-Body Reach: Use your good arm to pull the affected arm across your chest. Hold for 15 to 30 seconds.
- Wall Climb: Stand facing a wall. Use your fingers to walk up the wall as high as you can.
- Doorway Stretch: Stand in a doorway. Place your arms on the frame and lean forward to stretch.
Perform these exercises at least three times a week. Start slowly and increase the intensity gradually. Always consult a physical therapist for a personalized plan.
Lifestyle Modifications
Making certain lifestyle changes can improve outcomes. Simple adjustments can ease discomfort and enhance mobility. Consider these tips:
- Maintain a Healthy Weight: Excess weight can increase strain on joints.
- Stay Active: Engage in low-impact activities, like walking or swimming.
- Apply Heat or Cold: Use heat pads or ice packs to relieve pain.
- Practice Good Posture: This helps reduce pressure on the shoulder.
Monitor blood sugar levels closely. This is crucial for overall health. Discuss your progress with your healthcare provider regularly.

Credit: www.e-dmj.org
Medications And Treatments
Managing Adhesive Capsulitis in people with Diabetes Mellitus involves specific medications and treatments. These help reduce pain and improve joint mobility. Understanding your options is key to better joint health.
Anti-inflammatory Drugs
Anti-inflammatory drugs are often the first line of treatment. They help reduce swelling and pain. Common types include:
- Nonsteroidal anti-inflammatory drugs (NSAIDs)
- Corticosteroids
These medications can be taken orally or injected. Here’s a quick overview:
| Drug Type | Usage | Potential Side Effects |
|---|---|---|
| NSAIDs | Pain relief, inflammation reduction | Stomach upset, headache |
| Corticosteroids | Reduce severe inflammation | Weight gain, mood changes |
Consult a doctor before starting any medication. They can help choose the right drug based on your health needs.
Insulin Therapy And Joint Health
Insulin therapy is crucial for managing diabetes. Maintaining stable blood sugar levels can improve joint health. High blood sugar can worsen Adhesive Capsulitis symptoms.
Consider these points:
- Regular monitoring of blood sugar levels
- Adjusting insulin doses as needed
- Following a balanced diet
Good diabetes management may speed up recovery from joint pain. Work with healthcare providers to ensure optimal treatment plans.
Surgical Interventions
Surgical interventions for adhesive capsulitis in patients with diabetes mellitus can help restore movement. These procedures aim to reduce pain and improve shoulder function. Two common surgical options are:
- Arthroscopic Release
- Manipulation Under Anesthesia
Arthroscopic Release
Arthroscopic release is a minimally invasive procedure. Surgeons use small incisions to insert a camera and tools. This allows them to see and treat the affected area directly.
Benefits of arthroscopic release include:
- Less pain post-surgery
- Quicker recovery time
- Reduced scarring
During the procedure, the surgeon:
- Inserts a small camera (arthroscope) into the shoulder joint.
- Identifies tight ligaments and inflamed tissue.
- Removes or releases these tissues.
This helps to free the shoulder and improve movement.
Manipulation Under Anesthesia
Manipulation under anesthesia is another option. This procedure involves moving the shoulder while the patient is asleep. The goal is to break up adhesions in the joint.
Key points about this method:
- Quick procedure, often done in an outpatient setting.
- Immediate improvement in shoulder movement.
- May require physical therapy afterward.
During this procedure, the doctor:
- Administers anesthesia to the patient.
- Carefully moves the arm in various directions.
- Helps to stretch and break up the stiff tissue.
Both surgical options can be effective for managing adhesive capsulitis. They help improve quality of life for those with diabetes.

Credit: www.sciencedirect.com
Alternative Therapies
Alternative therapies offer various options for managing Adhesive Capsulitis in people with Diabetes Mellitus. These treatments can help reduce pain and improve mobility. Many individuals seek natural methods to ease discomfort. Here are two popular therapies: acupuncture and herbal supplements.
Acupuncture And Joint Pain
Acupuncture is an ancient practice from China. It involves inserting thin needles into specific points on the body. This therapy aims to balance energy and promote healing. Research shows acupuncture may help reduce joint pain linked to adhesive capsulitis.
Benefits of acupuncture include:
- Reducing pain and inflammation
- Improving joint mobility
- Enhancing overall well-being
Consult with a licensed acupuncturist. They can design a treatment plan tailored to your needs. Always inform them about your diabetes and any other health conditions.
Herbal Supplements
Herbal supplements can support joint health. Some herbs have anti-inflammatory properties. They may help ease pain and stiffness. Here are a few popular options:
| Herb | Benefits |
|---|---|
| Turmeric | Contains curcumin, an anti-inflammatory compound. |
| Ginger | May reduce pain and improve mobility. |
| Boswellia | Supports joint health and reduces inflammation. |
Always consult a healthcare provider before starting any herbal supplement. Some herbs may interact with diabetes medications. Proper guidance ensures safety and effectiveness.
Role Of Diet In Managing Symptoms
Diet plays a vital role in managing the symptoms of Adhesive Capsulitis in people with Diabetes Mellitus. Eating the right foods can help reduce inflammation and improve overall health. A balanced diet can support better blood sugar control and enhance recovery.
Anti-inflammatory Foods
Incorporating anti-inflammatory foods can help manage pain and stiffness. These foods fight inflammation and promote healing. Here are some key options to consider:
- Fatty Fish: Salmon, mackerel, and sardines are rich in omega-3 fatty acids.
- Leafy Greens: Spinach, kale, and collard greens are packed with antioxidants.
- Berries: Blueberries, strawberries, and raspberries are great for reducing inflammation.
- Nuts: Walnuts and almonds provide healthy fats and proteins.
- Olive Oil: Extra virgin olive oil is a healthy fat choice.
- Turmeric: Contains curcumin, known for its anti-inflammatory properties.
Dietary Tips For Diabetics
Managing diabetes while dealing with adhesive capsulitis requires careful planning. Here are some dietary tips to help:
- Control Portion Sizes: Smaller portions help manage blood sugar levels.
- Choose Whole Grains: Opt for brown rice, quinoa, or whole wheat bread.
- Limit Sugary Foods: Avoid candy, sodas, and desserts high in sugar.
- Stay Hydrated: Drink plenty of water throughout the day.
- Monitor Carbohydrate Intake: Balance carbs with protein and fats.
Eating a diet rich in whole foods can improve overall health. Pay attention to how different foods affect your symptoms. Consult a healthcare provider for personalized advice. Managing diet can lead to better symptom control and improved quality of life.
Innovations In Pain Management
Pain management for Adhesive Capsulitis in patients with Diabetes Mellitus is evolving. New methods aim to reduce pain and improve movement. Research and therapies are changing how we treat this condition. Patients can find relief through these innovations.
Latest Research Findings
Recent studies show promising results in pain management for adhesive capsulitis. Research focuses on understanding the condition better. Here are some key findings:
- Physical therapy improves shoulder mobility.
- Corticosteroid injections reduce inflammation effectively.
- Ultrasound-guided injections increase accuracy and effectiveness.
Studies also suggest that diabetes management may influence treatment outcomes. Controlling blood sugar levels can help improve recovery. Many patients report less pain and better movement when their diabetes is managed well.
Emerging Therapies
New therapies are being explored for adhesive capsulitis. These treatments aim to provide better pain relief. Some of these therapies include:
| Therapy | Description |
|---|---|
| Cryotherapy | Uses cold temperatures to reduce pain and swelling. |
| Platelet-rich plasma (PRP) | Involves injecting growth factors to promote healing. |
| Transcutaneous electrical nerve stimulation (TENS) | Uses electrical impulses to relieve pain. |
These therapies show potential for improving pain management. Patients should discuss options with their healthcare providers. Personalized treatment plans can lead to better outcomes. Each patient’s experience can differ based on their needs and conditions.
Patient Stories And Experiences
Hearing from real patients sheds light on Adhesive Capsulitis and Diabetes Mellitus. Their stories show the struggles and triumphs faced. Understanding their experiences helps others in similar situations.
Real-life Challenges
Patients with Adhesive Capsulitis often face many obstacles. Here are some common challenges:
- Pain: Constant pain limits daily activities.
- Stiffness: Moving the shoulder becomes difficult.
- Emotional Impact: Frustration and anxiety can arise.
- Limited Mobility: Everyday tasks like dressing are hard.
Many patients share their stories of struggle. For example, Sarah, a 45-year-old teacher, felt intense pain. She found it hard to raise her arm. Simple tasks like writing on the board became tough.
John, a 60-year-old mechanic, experienced similar issues. He couldn’t lift tools or reach for parts. His work suffered. Both Sarah and John felt alone in their journeys.
Success Stories In Management
Despite the challenges, many patients find ways to cope. They share their success stories, inspiring others. Here are some strategies that worked for them:
| Strategy | Description |
|---|---|
| Physical Therapy | Regular sessions improved flexibility and reduced pain. |
| Medication | Anti-inflammatory drugs helped manage pain. |
| Exercise | Gentle exercises maintained mobility and strength. |
| Support Groups | Sharing experiences offered emotional support. |
For instance, Sarah joined a physical therapy group. She learned exercises to regain movement. Over time, her pain lessened, and she felt stronger. John also found success through therapy. He adapted his work tasks and learned to manage pain effectively.
These stories show that recovery is possible. With the right support and strategies, patients can regain control over their lives.
Physical Activity Guidelines
Physical activity is essential for managing Adhesive Capsulitis and Diabetes Mellitus. It helps improve joint mobility and control blood sugar levels. Safe exercises can reduce pain and enhance overall well-being. Follow these guidelines to stay active and healthy.
Safe Exercises For Diabetics
Choosing the right exercises is crucial. Here are some safe exercises for diabetics:
- Walking: A simple and effective way to stay active.
- Swimming: Low-impact and easy on the joints.
- Cycling: Great for building strength without stress.
- Stretching: Improves flexibility and reduces stiffness.
- Yoga: Enhances balance and relaxation.
Each exercise should be done at a comfortable pace. Start with 10-15 minutes and gradually increase the duration. Always listen to your body. Stop if you feel pain.
Avoiding Further Injury
Preventing injuries is vital. Follow these tips:
- Consult a doctor: Get a check-up before starting any exercise program.
- Warm-up: Always begin with light stretches to prepare your body.
- Use proper form: Avoid straining muscles and joints.
- Stay hydrated: Drink water before, during, and after exercise.
- Take breaks: Rest if you feel tired or sore.
Listening to your body is key. If you have any concerns, seek advice from a healthcare professional. Stay safe while being active.
Coping Strategies For Chronic Pain
Living with adhesive capsulitis and diabetes mellitus can cause chronic pain. Finding ways to manage this pain is essential. Many strategies can help improve quality of life. Here are some effective coping strategies.
Mental Health Considerations
Chronic pain often leads to emotional challenges. Feelings of anxiety and depression may arise. Taking care of mental health is crucial for overall well-being.
- Practice Mindfulness: Focus on the present moment. Mindfulness can reduce stress.
- Engage in Relaxation Techniques: Try deep breathing or meditation. These methods can help calm the mind.
- Keep a Journal: Writing down thoughts can provide relief. It helps to express feelings and track pain levels.
Seeking professional help is important. A therapist can provide coping strategies. Supportive therapy can improve mental health.
Support Groups And Counseling
Connecting with others can ease feelings of isolation. Support groups offer shared experiences and advice. They help individuals feel less alone in their journey.
- Find Local Support Groups: Look for groups in your area. Many communities have resources available.
- Online Support Groups: These groups provide flexibility. They allow you to connect from home.
- Counseling Services: Professional counselors can guide you. They offer strategies tailored to your needs.
Support networks are vital. They provide emotional comfort and practical advice.
Insurance And Cost Considerations
Understanding the costs of Adhesive Capsulitis is vital. This condition often affects those with Diabetes Mellitus. Insurance coverage can vary greatly. Knowing your options helps manage expenses.
Covering Treatment Expenses
Insurance plans may cover some treatment costs. Check your policy carefully. Here are key points to consider:
- Physical therapy sessions
- Diagnostic tests like X-rays
- Medications prescribed for pain relief
- Surgery if needed
Always ask about co-pays and deductibles. Some insurance plans may require pre-approval for certain treatments. Understanding your out-of-pocket costs can save you money.
Financial Aid And Resources
Many resources help with treatment costs. Check local and national programs. Here are some options:
| Resource | Description |
|---|---|
| Nonprofit Organizations | Offer financial support for medical treatments. |
| Government Programs | Medicaid and Medicare may cover treatments. |
| Community Health Clinics | Provide services on a sliding scale. |
| Payment Plans | Some clinics offer payment options for treatments. |
Researching these options can ease financial stress. Don’t hesitate to reach out for help. Support is available for those facing Adhesive Capsulitis and related expenses.
Preventing Adhesive Capsulitis Recurrence
Preventing the recurrence of Adhesive Capsulitis is crucial for people with Diabetes Mellitus. This condition causes stiffness and pain in the shoulder. Those with diabetes are at a higher risk. Understanding prevention methods can help maintain shoulder health.
Maintaining Joint Mobility
Keeping your shoulder joint flexible is key. Regular exercises can improve mobility. Here are some effective methods:
- Stretching: Gentle shoulder stretches help maintain flexibility.
- Range-of-motion exercises: Perform these daily to keep the joint active.
- Physical therapy: A professional can guide you through tailored exercises.
Focus on these stretches:
| Exercise | Description |
|---|---|
| Cross-body stretch | Pull one arm across your body with the other arm. |
| Wall climb | Use your fingers to climb a wall slowly. |
| Pendulum swings | Lean forward and let your arm swing freely. |
Long-term Management Strategies
Effective long-term management can prevent recurrence. Consider these strategies:
- Regular check-ups: Visit your doctor for routine evaluations.
- Control blood sugar: Keep diabetes well-managed to reduce risks.
- Avoid repetitive motions: Limit activities that stress the shoulder.
Implement these lifestyle changes:
- Healthy diet: Eat a balanced diet rich in nutrients.
- Stay active: Engage in low-impact exercises regularly.
- Rest: Allow your body to recover after activity.
By maintaining joint mobility and following long-term strategies, you can significantly reduce the risk of adhesive capsulitis recurrence.
The Role Of Healthcare Providers
Healthcare providers play a crucial role in managing Adhesive Capsulitis associated with Diabetes Mellitus. They offer valuable support to patients. Their expertise guides effective treatment plans. This approach improves patient outcomes and quality of life.
Interdisciplinary Care Approach
An interdisciplinary care approach is essential. It involves various healthcare professionals. Each contributes unique skills to patient care.
- Primary Care Physicians: They diagnose and manage overall health.
- Physical Therapists: They design exercise programs to improve mobility.
- Endocrinologists: They manage diabetes effectively to reduce complications.
- Occupational Therapists: They help patients adapt daily activities.
This team works together. They create a comprehensive treatment plan. Regular communication is vital for success. Patients receive personalized care that addresses all aspects of their health.
Patient Education And Support
Education is key for patients with Adhesive Capsulitis. Providers must explain the condition clearly. Patients should understand their symptoms and treatment options.
- Teach about Adhesive Capsulitis:
- What it is.
- How it relates to diabetes.
- Common symptoms.
- Discuss treatment methods:
- Physical therapy.
- Medications.
- Surgery, if necessary.
- Encourage self-management:
- Exercise regularly.
- Monitor blood sugar levels.
- Follow dietary recommendations.
Support groups can also help. They provide a sense of community. Patients can share experiences and coping strategies. This support strengthens emotional health during recovery.
Monitoring Progress And Outcomes
Monitoring progress and outcomes in Adhesive Capsulitis with Diabetes Mellitus is crucial. Regular checks help assess treatment effectiveness. Tracking symptoms can guide adjustments in care plans. This ensures better management of the condition.
Tracking Treatment Efficacy
To track how well treatments are working, consider these methods:
- Keep a pain diary. Note pain levels daily.
- Record range of motion. Measure shoulder movement weekly.
- Use questionnaires. Evaluate daily activities and overall function.
A simple table can help summarize findings:
| Date | Pain Level (1-10) | Range of Motion (degrees) | Daily Activities Score (1-5) |
|---|---|---|---|
| Week 1 | 7 | 30 | 2 |
| Week 2 | 5 | 45 | 3 |
| Week 3 | 3 | 60 | 4 |
This tracking helps identify trends. A decrease in pain or improvement in movement shows progress.
Adjusting Care Plans
Adjusting care plans is essential for effective treatment. Use collected data to make informed changes. Here are some strategies:
- Consult with healthcare providers regularly.
- Modify physical therapy routines based on progress.
- Change medications if pain persists.
Make necessary adjustments based on individual needs. Continuous evaluation leads to better outcomes. Stay proactive in managing symptoms.
Future Directions In Treatment
Adhesive capsulitis is a common condition in people with diabetes. Finding better treatments is crucial. Research is ongoing to improve care and outcomes for patients. This section discusses potential advances and current research.
Potential Advances In Care
New methods may help treat adhesive capsulitis in diabetic patients. These methods focus on:
- Physical Therapy: Tailored programs can improve mobility.
- Medications: New pain relief options may become available.
- Steroid Injections: Better techniques can enhance effectiveness.
- Minimally Invasive Surgery: Less invasive options may reduce recovery time.
Technology plays a role too. Wearable devices can track progress. Apps may provide reminders for exercises. Virtual reality may assist in rehabilitation.
Ongoing Research In Diabetic Complications
Researchers are studying the link between diabetes and adhesive capsulitis. Key areas of focus include:
- Inflammation: Understanding how inflammation affects the shoulder.
- Blood Sugar Control: Examining how glucose levels impact healing.
- Genetics: Investigating genetic factors that increase risk.
| Research Focus | Potential Impact |
|---|---|
| Inflammation | Targeted therapies for pain relief |
| Blood Sugar Control | Improved recovery strategies |
| Genetics | Personalized treatment plans |
These research efforts aim to improve treatment for adhesive capsulitis. Better understanding leads to better care.
Credit: theprehabguys.com
Frequently Asked Questions
What Is Adhesive Capsulitis?
Adhesive capsulitis, also known as frozen shoulder, is a condition that causes stiffness and pain in the shoulder joint.
How Is Adhesive Capsulitis Related To Diabetes?
People with diabetes often have a higher risk of developing adhesive capsulitis due to changes in collagen and blood sugar levels.
What Are The Symptoms Of Adhesive Capsulitis?
Common symptoms include shoulder pain, limited range of motion, and difficulty with daily activities.
How Is Adhesive Capsulitis Diagnosed?
A doctor typically diagnoses adhesive capsulitis through a physical exam and by reviewing medical history.
What Are The Treatment Options For Adhesive Capsulitis?
Treatment may include physical therapy, medications, and sometimes injections or surgery for severe cases.
Can Adhesive Capsulitis Go Away On Its Own?
Yes, adhesive capsulitis can resolve on its own, but it may take months to years.
How Long Does Adhesive Capsulitis Last?
The condition can last from several months to a few years, depending on treatment and individual factors.
Is Adhesive Capsulitis Common In Diabetes?
Yes, adhesive capsulitis is more common in people with diabetes compared to those without it.
What Can Increase The Risk Of Adhesive Capsulitis?
Risk factors include diabetes, shoulder injuries, and prolonged immobility of the shoulder.
Can Lifestyle Changes Help Prevent Adhesive Capsulitis?
Maintaining a healthy lifestyle, managing blood sugar, and staying active can help reduce the risk.
Conclusion
Adhesive capsulitis can be a tough challenge for those with diabetes. Pain and stiffness in the shoulder can limit daily activities. Understanding this condition is key. Early diagnosis helps manage symptoms better. Simple treatments like physical therapy can make a difference.
Staying active is important for overall health. Always consult a healthcare provider for guidance. With the right care, patients can find relief and improve their quality of life. Don’t ignore the signs. Take steps to address shoulder pain early. Your health matters.